Three decades after Iraq unleashed chemical weapons on Iran, scientists there are unraveling the long-term effects.
Halabja, 17 March 1988: Iraq attacked its own citizens with nerve agents. During its war with Iran, enemy soldiers and civilians were frequent targets.
On a chilly morning in September 1987, in the waning days of the Iran-Iraq War, an 18-year-old Iranian soldier named Seyed Naser Emadi drove from a battlefield in northwestern Iran to a hospital in Nagadeh, a city a couple hours away. Crammed in the back of his Land Rover were four soldiers, moaning, vomiting, and coughing. "I'll never forget the sound of their breathing,” Emadi says. "It was rattling, raspy.” The terrified young men did not know what was happening, and Emadi had no idea how to help them.
They complained about the cold, so Emadi rolled up his window. The air in the vehicle became stifling, and a strong chemical odor wafted from the men's uniforms. Emadi grew nauseous and dizzy, but he made it to the hospital. There, he tried to rouse the nearest victim, whose face and hands had large blisters. The young man would not wake up. As Emadi and a hospital aide carried the victim out of the vehicle, a blister on the man's arm burst, and fluid splattered on the back of Emadi's hand. A couple hours later, he felt a burning sensation and his own hand began to blister.
The experience set Emadi on the path to becoming a medical researcher. (He is now a dermatologist at Tehran University of Medical Sciences and a volunteer with Doctors Without Borders.) It also highlighted one of the cruelest practices in the 1980–88 conflict, which also featured child soldiers and trench warfare. For the first time ever on a battlefield, nerve agents including sarin and tabun were unleashed by Iraqi forces. "These are the most toxic chemical warfare agents ever developed,” says Jonathan Newmark, a neurologist in Burke, Virginia, who has helped develop countermeasures against such weapons at the U.S. Army Medical Research Institute of Chemical Defense (USAMRICD) in Edgewood, Maryland, and other agencies. And on scores of occasions, Iraq shelled soldiers and villagers with sulfur mustard—the chemical that afflicted Emadi and his passengers.
After the war, Iraq—pressured to own up to the attacks—acknowledged that it had "consumed” 1800 tons of mustard, 600 tons of sarin, and 140 tons of tabun. All told, according to Iran's Foundation of Martyrs and Veterans Affairs (FMVA), the chemical onslaught killed nearly 5000 Iranians and sickened more than 100,000. That doesn't include Iraqi victims: In March 1988, Iraq's forces attacked its own citizens with mustard and nerve agents in Halabja, killing as many as 5000 and wounding 7000.
Seyed Naser Emadi as a teenage soldier in the Iran-Iraq War, where he witnessed chemical attacks, and at a meeting of survivors in Tehran last October.
PHOTOS (TOP TO BOTTOM): SEYED NASSER EMADI; EBRAHIM MIRMALEK
Sulfur mustard, a family of compounds first used in World War I, left the deepest and most visible scars on survivors of the war. Three decades later, about 56,000 Iranians are coping with lingering health effects from the blistering agent, ranging from skin lesions and failing corneas to chronic obstructive lung disease and possibly cancer, says Tooba Ghazanfari, an immunologist at Shahed University here.
The scale of the atrocities means that Iran has a unique opportunity to study the long-term effects of chemical weapons. Ghazanfari is leading an effort at a dozen research centers across Iran to uncover how wartime mustard exposures wreaked molecular mayhem that, decades later, triggers illnesses and death. "I'm pretty amazed about the scale of exposures and how many people have been followed,” says neuroscientist David Jett, director of the Countermeasures Against Chemical Threats (CounterACT) Program at the U.S. National Institutes of Health in Bethesda, Maryland, which is spearheading R&D on several promising methods of neutralizing such agents (see sidebar, p. 23).
The data, some of which are beginning to appear in Western journals, have unavoidable limitations. The Iranian researchers can only estimate the doses that victims absorbed, and complicating the picture is the fact that Iraqi forces sometimes attacked with mustard and nerve agents simultaneously. "That makes it really difficult to determine what's going on,” says James Madsen, a physician and lead clinical consultant in USAMRICD's Chemical Casualty Care Division. Still, U.S. researchers say the Iranian findings are pointing to new molecular targets for treating mustard's long-term effects.
So far, Iran has not undertaken a similar study of nerve agent survivors, who also number in the thousands. Based on Japanese victims of sarin attacks by the Aum Shinrikyo doomsday cult in the mid-1990s and U.S. soldiers possibly exposed to sarin in Iraq, researchers suspect that nerve agents leave a legacy of neurological damage. But chemical weapons experts have struggled to link sarin to specific chronic symptoms; they are hoping for some clarity from a U.S. review that is about to be released. And Iranian researchers say they may start their own probe of nerve agents' long-term health effects. "We want to get the knowledge out,” says Mohammad-Reza Soroush, a physician here at the Janbazan Medical and Engineering Research Center.
Ali Reza Yazdanpanah holds up a photo of himself after he was exposed to sulfur mustard during the Iran-Iraq War. Now a docent at the Tehran Peace Museum, he calls the repeated use of chemical weapons against his nation "Iran's Hiroshima.”
PHOTO: EBRAHIM MIRMALEK
WITH HIS BEARISH FRAME and thick black beard, Ali Cherchi would be an imposing figure—if he weren't propped up in a hospital bed with an oxygen tube in his nose and an intravenous line plying him with antibiotics. His infection-riddled lungs are giving out.
Like many teenage boys filled with patriotic fervor during the war, Cherchi lied about his age, saying he was 18 instead of 17 so he could enlist in the army. One day in 1986, near the Persian Gulf in southern Iran, the Iraqis shelled his 200-strong platoon with mustard and tabun. Many of the young men had beards, so their gas masks did not fit tightly. "I felt like I was suffocating,” Cherchi says. Only a few dozen survived the attack, and since then most of the rest have died. "I'm the champion for having lasted so long,” he says with an ironic laugh.
For years, Cherchi indeed considered himself fortunate: He studied law, married, and had children. But now, a short stroll can leave him gasping for breath. Lung infections land him for weeks at a stretch here at Sasan Hospital, Iran's premier facility for chemical weapons victims, which treats as many as 150 such patients on any given day. As Cherchi tells his life story in a hospital ward, his confident voice falters and, eyes widening, he reaches for an inhaler. "Chemical weapons are not fair,” he says.
An old scourge ruined Cherchi's lungs. Called mustard because of its odor and the enormous yellowish blisters, or bullae, that it forms on the skin, bis(2-chloroethyl) sulfide—the primary member of a family of noxious compounds—debuted on the battlefield in July 1917, when Germany used it against U.K. and Canadian soldiers near Ypres, Belgium. After a mustard-filled artillery shell detonates, the chemical is dispersed as fine droplets that settle to the ground. In hot and dry climates, mustard can vaporize and is more likely to be inhaled. A mere 7 grams—a teaspoonful—is a lethal dose, Madsen says.
How the mustards produce their acute effects is well known. The oily liquid dissolves readily in fat, allowing it to penetrate skin. Inside cells, the chemical corrupts DNA and proteins. Recovery from the tissue damage can take months, and some World War I mustard survivors succumbed years later to respiratory failure.
Countries stockpiled sulfur mustard during World War II, but it saw limited use in battle. However, thousands of workers in a weapons factory on Ōkunoshima, an island in Japan, were exposed to mustard on the job. Studies flagged an elevated lung cancer risk, but failed to shed light on the mechanism of sulfur mustard's long-term effects, says pharmacologist Jeffrey Laskin, who directs a CounterACT center on chemical weapons countermeasures at Rutgers University's Robert Wood Johnson Medical School in Piscataway, New Jersey.
Iranian scientists are seeking answers. A decade ago, Ghazanfari and colleagues launched the Sardasht-Iran cohort study, named after a town in the northwest part of the country that was the site of one of the war's more reprehensible acts.
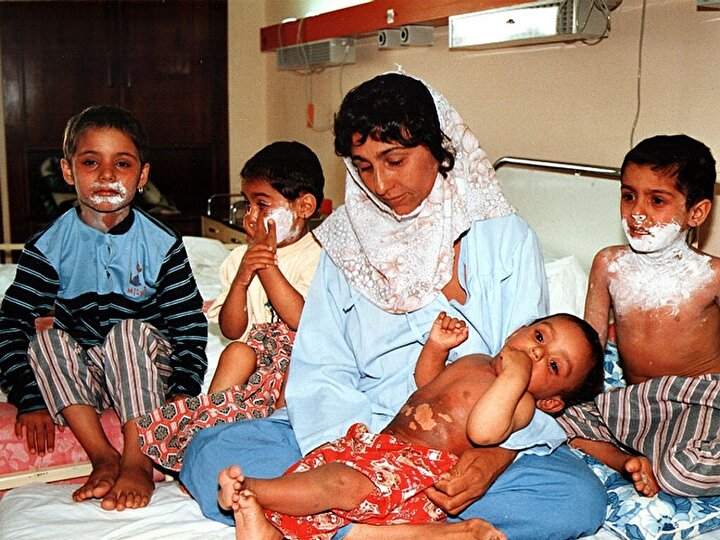
On 28 June 1987, Iraqi aircraft dropped four 250-kilogram bombs filled with mustard on residential areas of Sardasht. "It was a completely innocent city,” says Mohammad-Reza Vaez Mahdavi, a Shahed University physiologist who studies the survivors. Records show that 8025 of the 12,000-odd residents were exposed. A few dozen—mostly children and elderly—died within hours or days. About 1500 people suffered moderate to severe symptoms, and at least 100 have since succumbed to respiratory failure, Ghazanfari says.
With funding from FMVA, Ghazanfari's team is tracking the health of 850 male victims, now aged 30 to 70. Most still reside in Sardasht. For a control group, the scientists recruited 150 men of equivalent age in Rabat, a village 15 kilometers from Sardasht. During the war, Rabat was shelled often—but never with chemical weapons. "Both populations endured a lot of stress,” Ghazanfari says. In principle, that allows her team to zero in on illnesses in Sardasht that can't be chalked up to stress or factors such as diet and economic status, which are similar in Sardasht and Rabat.
The Sardasht survivors have much higher rates of eye and skin disorders. A few have also developed cutaneous T-cell lymphoma at the site of old mustard burns. Emadi says the uncommon skin cancer may also explain mysterious lesions that doctors in the early 20th century noted in World War I mustard victims. But he says that benign skin lesions are far more common in the victims: patches that lack sweat glands or the ability to secrete sebum, resulting in intensely itchy, dry skin that's susceptible to infection.
IT'S IN THE LUNGS where mustard wreaks the most havoc. "Many soldiers on the battlefield don't have symptoms, but years later they come to us with problems,” says Mostafa Ghanei, a physician at Baqiyatallah University of Medical Sciences here who consults for the Organisation for the Prohibition of Chemical Weapons (OPCW) in The Hague, Netherlands. Mustard creates what he calls a "unique pathology”: peribronchial fibrosis—a thickening in tissues surrounding the bronchi—coupled with an airway obstruction called bronchiolitis obliterans.
To get at the roots of these symptoms, the Iranian team is probing a complex cascade of biochemical perturbations that persists in mustard survivors. They have detected, for example, revved up signaling molecules involved in inflammation, such as tumor necrosis factor α (TNFα) and other cytokines; skewed populations of natural killer cells and other immune cells; imbalances in the protein-destroying enzymes called proteases; and a shortening of the telomeres, the "end caps” on chromosomes, which indicates prematurely aged cells.
"They're doing a really good job documenting what's going on,” Laskin says. But why the cellular dysfunction occurs decades after exposure is still a puzzle, he adds.
DNA methylation and other epigenetic alterations—chemical changes to DNA that can alter a gene's expression without affecting its protein-coding sequence—may underlie some of the lasting biochemical havoc, Ghanei says. He and colleagues have found evidence, for example, that methylation of tumor suppressor genes may inactivate them and help explain the development of peribronchial fibrosis as well as slightly elevated rates of certain cancers, in particular blood cancers.
In the past, Ghanei says, mustard victims with chronic symptoms were given standard treatments for chronic pulmonary disorders such as asthma: corticosteroids to tamp down inflammation and β2-agonists for smooth muscle relaxation. He and his colleagues now view oxidative stress as a prime target, because levels of an important antioxidant and an enzyme that scavenges destructive free radicals are suppressed in mustard victims. Iranian doctors now treat chronic mustard patients with antioxidants such as N-acetylcysteine, which alleviates the frequency and severity of bronchiolitis attacks, Ghanei has found.
Researchers in the United States are exploring other potential treatments. Drugs that neutralize TNFa might help, Laskin says. Another promising lead came when pediatric pulmonologist Livia Veress of the University of Colorado in Denver and colleagues zeroed in on fibrin clots in rats exposed to mustard. When she dissected the animals, she pulled out of their lungs white clots called casts that looked like "tree branches,” she says. "I realized I'd seen that before”—in children with plastic bronchitis, a rare complication of surgery to repair congenital heart defects. Veress tested a clot-busting drug, tissue plasminogen activator (tPA), in rats exposed to normally lethal mustard doses—they all survived. Her team has since given tPA to seven children with plastic bronchitis, which normally has a mortality rate of up to 60%. "These are really sick kids,” she says. All survived; other hospitals have treated 22 children, all of whom recovered, too. "It's pretty darn cool,” Veress says. Her team is working toward U.S. Food and Drug Administration (FDA) approval for tPA's use for plastic bronchitis and next month, they will start testing the drug in pigs to further demonstrate its potential as a sulfur mustard treatment.
Those prospects, although tantalizing, are still on the horizon, and mustard remains a grave concern: In March 2016, the Islamic State group shelled a village in Iraq near Kirkuk with rockets filled with mustard. "It is just as much of a threat now as it was in the Iran-Iraq War,” Madsen says.
THAT IS EQUALLY TRUE for the nerve agents, which many nations still stockpile and which were used as recently as last April against civilians and rebel soldiers in Syria.
Syed Abbas Foroutan remembers their grim debut. In March 1984, he was a young army doctor running a unit for treating mustard victims when some soldiers with unusual symptoms were brought in. They were coughing and short of breath, and some were vomiting and drifting in and out of consciousness. It was clear to the doctors that they weren't dealing with mustard. "We could only say it was not this, not that,” Foroutan says—until he found a symptom common to all the victims: "Their pupils were constricted to pinholes.”
That pointed to a nerve agent. Such weapons form a covalent bond to and inactivate acetylcholinesterase (AChE), an enzyme that breaks down acetylcholine in synapses, thereby regulating levels of the neurotransmitter. A few days later, comatose victims started arriving to the clinic. Foroutan checked their AChE levels—they were near zero. The clincher was that the ill soldiers responded to atropine, which binds to and blocks acetylcholine receptors, reducing the effects of excess levels of the neurotransmitter. That realization was the beginning of a grave challenge for a young doctor fresh out of medical school, says Newmark, who has studied Foroutan's experiences. "He was the world's first physician to care for battlefield nerve agent casualties.”
Undeterred by charges that it was engaging in a war crime, Iraq repeatedly shelled Iranian forces with tabun, and later with sarin as well as a binary form of the agent, cyclosarin. As Iraqi chemists learned to synthesize nerve agents with fewer contaminants and the military became more adroit at delivering them, the attacks were deadlier. Some casualties went "from fully functioning to seizing and comatose in seconds,” Newmark says. Emadi, who witnessed such deaths, calls the victims "chemical martyrs.”
To cope with the more potent threat, Foroutan pumped afflicted patients with massive doses of atropine—up to 10 times the amount that the United States and the North Atlantic Treaty Organization advise, near the threshold where the drug itself becomes toxic. "Foroutan was doing the best he could with what he had,” Madsen says.
The radical treatment paid off, Newmark says. In most nerve agent fatalities, death occurs after the agent binds to enough AChE to block signal transmission from the brain's respiratory center to the diaphragm, paralyzing the muscle that's vital for breathing. "It takes fairly high doses of atropine to get into the brain,” Madsen says. "What Foroutan did was intuitive. He gave so much atropine, we think that it started to take care of the [central nervous system] effects.” Newmark puts it this way: "If a soldier got a snoot full of nerve agent, he was lucky to get to Foroutan's unit.”
But what happened in later years to Foroutan's patients—and to thousands of others who survived nerve agent attacks—is largely unknown. That frustrates researchers, who would like to follow up on hints that exposure takes a long-term toll.
One clue comes from an episode in the United States, during Prohibition, when doctors in New York City and elsewhere in the 1920s started seeing patients with muscle spasms, tingling and numbness in the legs, and, in some cases, paralysis. Medical sleuths eventually zeroed in on the cause: an adulterant, triorthocresyl phosphate, in a bootleg ginger liquor. That compound, like nerve agents, is an organophosphate, and the symptoms that afflicted the "Ginger Jake” drinkers—some 30,000 documented cases—are now known as organophosphate-induced delayed neurotoxicity (OPIDN). The same syndrome affected one victim of the Aum Shinrikyo cult's sarin terrorism, says Bahie Abou-Donia, a neurobiologist at Duke University in Durham, North Carolina. "It would not surprise me to see OPIDN in the Iranian survivors,” Madsen says.
There's firmer evidence, he says, that nerve agents mess with the mind. Studies of the Aum Shinrikyo survivors link exposure "even at really low doses” to symptoms such as nightmares, headaches, drowsiness, confusion, memory deficits, irritability, and depression—a syndrome called organophosphorus-ester-induced chronic neurotoxicity (OPICN). In March 1991, during the Gulf War, tens of thousands of U.S. soldiers may have been exposed to low doses of sarin after the destruction of an Iraqi ammunition dump, says Abou-Donia, a sarin expert. An unknown percentage of cases of the still-controversial Gulf War Syndrome, he says, may in fact be OPICN.
Female volunteers learning to use gas masks in a Tehran mosque in May 1988. In the waning days of the war, Iraq resorted more frequently to bombarding soldiers and civilians with sulfur mustard and nerve agents.
PHOTO: KAVEH KAZEMI/GETTY IMAGE
More clarity on the long-term effects of nerve agents will come from a U.S. National Toxicology Program report on sarin. The draft review concludes that sarin's chronic effects include AChE inhibition, vision and memory problems in people, as well as nerve pathology detailed in animal studies.
The Iranian veterans could yield a more definitive picture. "Whatever comes out of Iran on this,” Newmark says, "will be the best human data that exists.” But so far, no one is gathering it. After the war, Foroutan became a professor—he's now at Shahid Beheshti University of Medical Sciences here—and has not tracked his former patients. And zeroing in on late nerve agent effects is not simple. "We don't have reliable information on who was exposed solely to nerve agents,” says Janbazan medical researcher Batool Mousavi, because of the Iraqi practice of bombarding troops with nerve agents and mustard simultaneously or on consecutive days.
Foroutan believes that it's not too late to delve into the long-term consequences. "We need a Sardasht cohort for nerve cases,” he says. It could even be an international effort, Newmark suggests, if Iran were to set up a collaboration under OPCW's auspices. "It's important to know if neuropathology and resultant long-term effects actually occur in humans,” Jett adds, "before we approach the FDA for approval of a neuroprotectant drug.”
IN THE HEART OF TEHRAN, a modest one-story building is a living memorial to Iran's chemical weapons victims. Inside the Tehran Peace Museum, exhibits recount the global history of chemical warfare. Chemical victims of the Iran-Iraq War volunteer as docents. One is named Ali Reza Yazdanpanah.
When he was 15 years old, Yazdanpanah tricked his mother into signing his enlistment papers. Several weeks later, he and 31 other young men in his regiment were exposed to mustard near Khorramshahr, a port city on the Persian Gulf, near the Iraq border. Some of the blistering agent got in his eyes. "I lost my sight for some time,” he says. It came back, but he has had to endure four cornea transplantations, and is on a waiting list for a new pair of lungs. He says he has never felt completely well.
Yazdanpanah is keeping the memory alive. And as a subject in Iran's research efforts, he hopes his experience will benefit future victims of these ghoulish weapons. "The best years of my life,” he says, "were stolen from me.”
↵* Reporting for these stories was supported by the Pulitzer Center on Crisis Reporting.